Health: Health 4 Palestine (H4P)
Expanding Healthcare for Refugee Communities
Program: Health 4 Palestine
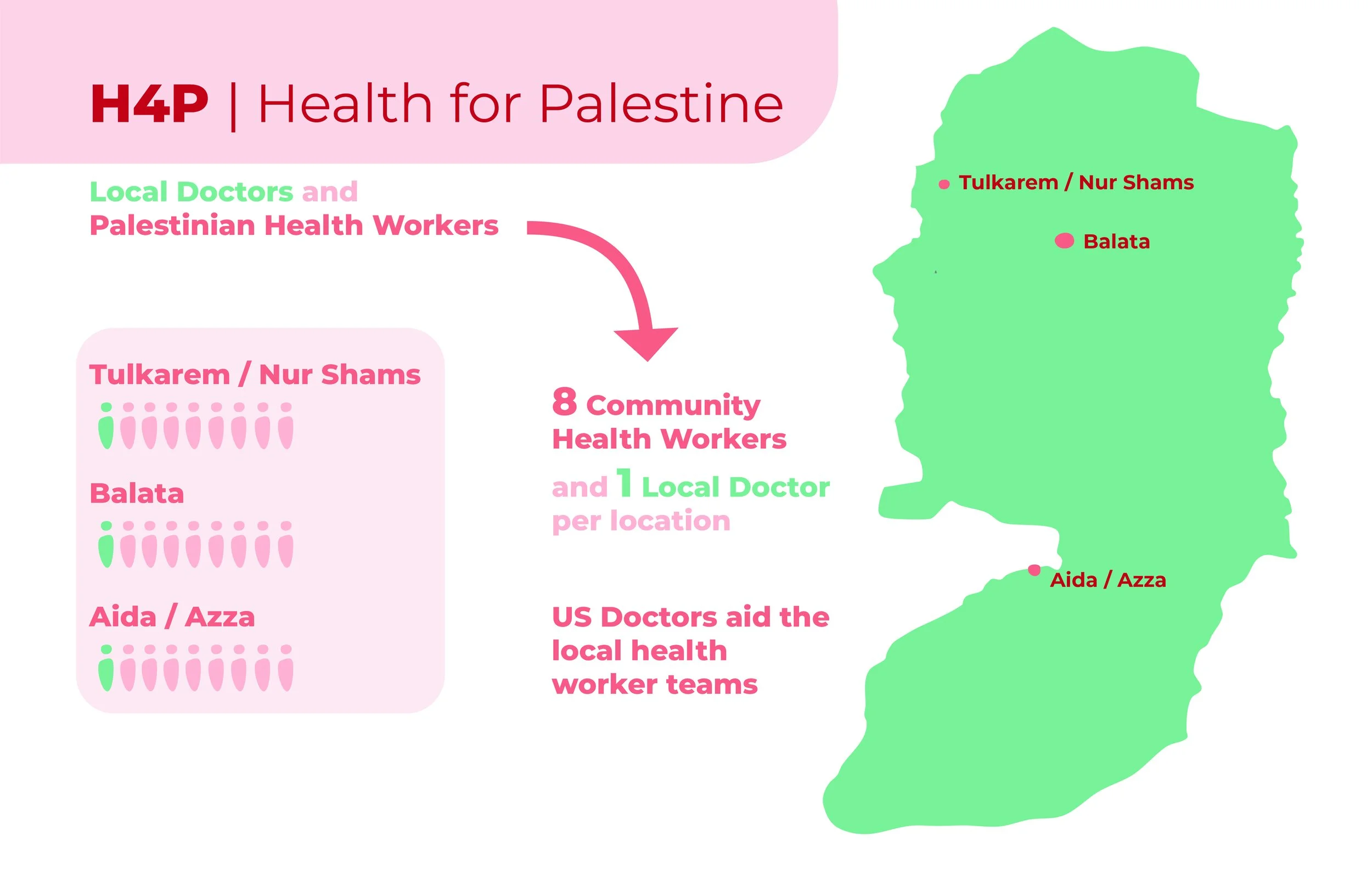
Health 4 Palestine (H4P) is a program that serves Palestinian refugees living in UN-run camps in the West Bank. It operates on a Community Health Worker (CHW) model that is uniquely Palestinian. 1for3 & its partner in the West Bank the Lajee Center, located in the UN-run Aida refugee camp, jointly direct & fund the program. H4P currently works in five UN-run camps, serving a total community of approximately 80,000 refugees.
For over six years the members of H4P have trained mixed gender teams of Palestinian young professionals to serve as CHWs in UN-run Palestinian refugee camps. This training provides skills, employment & supports public health improvement. The teams target patients suffering from chronic illnesses & mental trauma.
2024
Gained a new partner, Al-Awda Center, and two new camps, Tulkarm and Nur Shams.
Trialed a Pediatric Care Initiative in Balata and Aida camps, which will serve over 150 when up-and-running.
Conducted trainings of CHWs in emergency medicine by US and Palestine-based MDs, both in-person and virtually.
Led a fact-finding mission in November of health professionals and architects.
Increased patient numbers from 280 to over 700. The impact is far beyond these numbers as each patient aids other family members.
Conducted a Community Lifesaving Course in Aida and Balata camps with doctors from Boston Children’s and Harvard Humanitarian Initiative.
Planned our first physical health clinic in the UN-run Aida refugee camp.
Organized and ran medical days with international and local MDs to provide healthcare and education to hundreds of refugees during the year.
Community Need
H4P started in 2018 when our partners at the Lajee Center in the UN-run Aida refugee camp alerted us to a growing need for community-based physical and mental health solutions for chronically ill residents. After discussions with our partners in Palestine, and consultations with experts at Harvard Medical School, Cornell Medical School, and the University of Massachusetts Boston, H4P was born. H4P uses a service model pioneered in Haiti by Partners In Health (PIH).



H4P Leadership Team
-

Bram Wispelwey, MD
Co-Founder H4P
Associate Physician, Division of Global Health Equity, Brigham and Women’s HospitalInstructor, Harvard Medical School; Harvard T.H. Chan School of Public Health. He is a Co-founder and Chief Strategist of Health for Palestine. Dr. Wispelwey’s research focuses on structural racism in hospital triage, ethics, community health worker impact, social and political barriers to health, and colonial violence. Before his medical career, Dr. Wispelwey pursued LGBT-rights activism. He is currently an Atlantic Health Equity Fellow.
-

Henry Louis, MD
H4P International Medical Director
Family Medicine Resident Physician, University of Massachusetts Medical School. Dr. Louis's responsibilities include supervising all activities related to qualitative and quantitative data collection on program activities. Furthermore, alongside the team of international advisers, Dr. Louis contributes to a diverse array of development efforts including community organizing. His passion for working alongside community members and pursing health equity and social justice have dragged him across the world, from Egypt to Armenia to his current beloved Palestine.
-

Karameh Hawash Kuemmerle, MD
H4P Balata
Dr. Karameh is an assistant professor at Harvard Medical School and a pediatric neurologist at Boston Children’s Hospital. She specializes in traumatic brain injury and epilepsy.
Much of Dr. Karameh’s work takes place in the Brain Injury Center at Boston Children’s Hospital, a multidisciplinary center coordinating care between the Trauma Center, Neurology, Neurosurgery, Sports Medicine, and Neuropsychology.
-

David Scales, MD
Co-Founder H4P
Assistant Professor of Medicine, Medicine, Weill Cornell Medical College. He has extensive experience with various NGOs in the region, serving on the board of Questscope and having volunteered to provide medical assistance to Syrian refugees in Jordan. Trained in Sociology and Internal Medicine, his interests center on structural determinants of health, health disparities, and medical communication.
-
Aya Darwish, CHW
H4P Palestine Director
Aya has been a community Health worker since 2019. Darwish studied medical laboratory in Bethlehem and continue to study counseling and mental health with a team of local Palestinian and international phycologists.